The following is a white paper written by SurgiScreen, which provides consulting, management support and outsourcing of pre-surgical screening services.
Introduction to pre-surgical screening
The process of preparing a patient for a successful surgical procedure has evolved over many years alongside the evolution of surgery itself. Pre-surgical screening was developed with the view to not only increase efficiency for the surgical facility, but to improve patient care during and after a surgical procedure. Several studies show that a thorough medical history taken in advance of surgery leads to a reduction in morbidity caused by complications during surgery, a decrease in costs related to perioperative and postoperative care, and aids in a more rapid recovery for the patient.
Sometimes referred to as pre-surgical screening, pre-anesthesia testing or pre-anesthesia evaluation, the actual process varies as widely as the names prescribed to it. The process ranges from virtually no patient contact prior to the day of surgery to a comprehensive evaluation clinic where a patient receives a full physical and standard testing.
From a clinical perspective, the pre-surgical screening (PSS) process has more to do with the anesthesia administered during a surgical procedure than with the surgical procedure itself. Various pre-existing medical conditions can greatly increase the risk of surgery under anesthesia, so a comprehensive medical history will enable an anesthesiologist to reduce these risks. Frequently, the anesthesiologist will recommend specific diagnostic testing based on this information.
However, an efficient pre-surgical screening process has been shown to have significant impact on same day cancellation rates and late surgery starts which directly affects operational efficiency. Cancellation rates vary among facilities, depending partly on the types of patients receiving care. Typical rates range from 4.6 percent for outpatients, to 13 -18 percent at VA medical centers. Well functioning OR suites should have cancellation rates less than 5 percent.2
Revenues lost from cancellations range from $1,430 to $1,700 per hour plus variable costs in hospitals not on a fixed budget.3 It has been demonstrated that same day cancellations often occur because the patients are not sufficiently prepared for surgery and may not be fully aware of what to expect on the day of surgery, may have eaten prior to arrival, failed to discontinue medication, or failed to make arrangements for transportation home after surgery.
Many delays are due to assessments on the day leading to further laboratory tests being required before surgery. Since operating room costs range from $22-47 per minute at an average hospital, even small delays can be costly.1 If multiple delays occur throughout the day, overtime pay may also be incurred for operating room staff.
In addition to clinical and operational considerations, delays and cancellations can lead to frustration and dissatisfaction for the facility’s clinical staff as well as patients and surgeons. This leads to lower OR utilization and damages the institutions relationship with the community.
While the benefits of a good PSS process have been well documented, many institutions fail to recognize the impact the process has on their bottom line. In many cases, the pre-surgical screening process has remained essentially unchanged despite rising expectations for patient safety amid falling reimbursements. The vast majority of surgical facilities still use highly paid clinical staff to perform basic data-gathering and clerical tasks, an inefficient staffing model that greatly increases cost while failing to achieve some of the most basic goals of PSS. The data presented here will show that the future of pre-surgical screening lies in a balanced application of technology, lean business management and personal customer service from a highly trained staff.
Goals of an Effective Pre-Surgical Screening Process
The goals of an effective pre-surgical screening process are relatively straightforward:
- Improve patient safety by capturing patient health history in advance, accurately assess the results, and distribute the data to appropriate clinical staff when needed.
- Improve the efficiency of diagnostic testing by assuring that all necessary testing is completed prior to day of surgery while reducing the frequency of unnecessary or duplicative testing.
- Improve operational efficiency and staff satisfaction by reducing cancellations and delayed starts.
- Improve patient satisfaction by thoroughly and appropriately preparing the patient for surgery.
Current pre-surgical screening processes
The current state of the pre-surgical screening process offers a variety of approaches to the challenge, most of which can be gathered under one of three broad categories. At one end of the spectrum, the screening process is poorly defined and often conducted only on the day of surgery. At the other end of the spectrum, fully staffed stand-alone clinics screen up to 100 percent of surgical patients. Between these ends exists a variety of partially defined processes which are often under-funded and under-staffed. Let’s take a closer look at each of these categories.
1. No defined process, same day screening
Under this model, patients arrive at the hospital or clinic and are "triaged" upon arrival. A clinical staff member, frequently an RN, may collect the patient’s health history. If the results of this process lead the clinician to recommend additional diagnostic testing, this testing must be completed prior to surgery leading to frequent delays and cancellations.
While it can be argued that the cost of this approach is lower as staffing requirements are less, the true cost of this service is actually much higher once the "soft costs" of surgical delays and cancellations, customer and surgeon satisfaction and patient safety are factored in. Delaying final assessment until the day of surgery can result in reduced patient safety, increased operating room expenses as well as decreased operating room efficiency.3,4
2. Partially defined process
ASCs often fall into this category. Since ASCs typically handle less invasive surgery cases, the required anesthesia is also less extensive. Commonly, the PSS process relies on Registered Nurses calling patients between various clinical duties during normal business hours. Although this process yields slightly better results than no patient contact, it still has many drawbacks.
The most frequent complaints from surgical patients regarding the pre-surgical process is that they are either not contacted at all, or they play phone-tag with a nurse, who typically has the same work schedule as the patient. Once contact is made, spending 20-40 minutes relaying sensitive medical information and lists of medications from the workplace leaves the patient embarrassed, frustrated and inconvenienced.
In a study of pediatric patients, data from 5,031 patients scheduled for ambulatory surgery were collected. During phase I of the study, when phone calls were attempted only during business hours, nurses contacted 805 of 1662 (48 percemt) of patients' parents. The contact rate improved to 71 percent (2,403 of 3,369 patients) during phase II of the study, when phone calls were made in the evening, and parents were encouraged by the surgeons to call the ambulatory unit. The rate of postponed or canceled surgery among those who could not be screened was 14.8 percent. Among patients who were screened, it fell to 9.7 percent (P less than 0.001).12 Clearly, increasing the range of available patient contact hours or methods can improve OR efficiency and decrease the risk of same-day cancellation, but this adds scheduling and wage considerations. Further, using clinicians to gather lengthy health histories over the phone is both expensive and inefficient, especially if the process is inconsistent and ill-defined.
3. Full preoperative clinic
At the other end of the spectrum are full preoperative clinics. Effective patient evaluation in a preoperative clinic has been shown to increase efficient utilization of operating room resources.5 Preoperative clinic visits have been shown to improve patient satisfaction,6 reduce unnecessary testing and consultation,7,8 and decrease duration of hospital stay.9 Preoperative risk factors are effective predictors of hospital costs; therefore, preoperative intervention to reduce risk could lead to significant cost savings.10 Optimization of a patient’s medical condition before surgery has also been shown to decrease operating room cancellations and delays.4 These outcomes are usually achieved by taking a full medical history and assessment by a nurse, and a complete array of laboratory tests. The information is then reviewed by an anesthesiologist before the patient is declared ready for surgery.
Despite the many advantages of a full preoperative clinic, most facilities are simply unable to fund the high cost of implementing this process. The capital investment in space and equipment along with the cost of increased staff and enhanced coordination required for this level of service is out of reach for all but a few health care facilities.
There is also some supporting evidence that many of the preoperative tests performed in a pre-op clinic are not necessary for the majority of patients. According to the New England Journal of Medicine, between 60 and 70 percent of laboratory tests ordered prior to surgery are not necessary, if the physician’s history and physical examination is taken into account. Therefore, it can be argued that if a patient is healthy and is undergoing elective surgery, "[a] good history and physical examination followed by a review of a patient’s chart are undoubtedly the most important routine tests needed." 11
In a manual PSS system, diagnostic testing is frequently ordered based on the judgment of the RN interviewing the patient. The tests ordered may fail to satisfy the attending anesthesiologist requiring additional testing and delays.
Summary
Pre-surgical screening processes vary based on a facility’s willingness and ability to invest resources in the process. The models range from a same-day review of a smaller percentage of patients to a full preoperative clinic screening 100 percent of surgery patients. Studies have demonstrated that failure to implement an effective pre-surgical screening process leads to higher rates of same-day cancellations and late starts, incomplete & over-ordered testing, patient dissatisfaction and staff frustration. Clearly, the evidence suggests that today’s environment requires a re-thinking of how pre-surgical screening is managed.
The Future of Pre-Surgical Screening
A best practice model
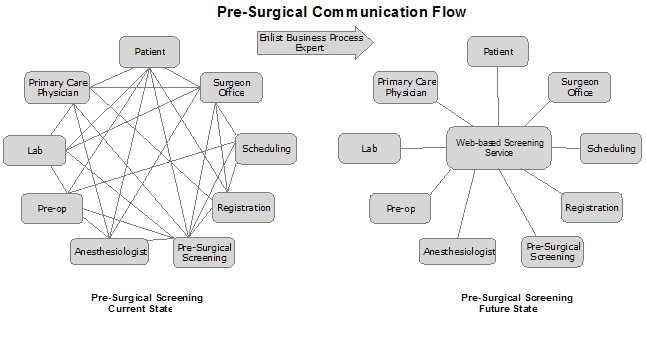
We believe that the future state of pre-surgical screening lies in leveraging web-based technology, intelligent systems, lean management techniques and customer-focused service. By breaking down the process into a series of steps aimed at effectively addressing each of the goals, we can begin to see a path to improving the efficacy and efficiency of the pre-surgical screening process.
First, make it easy and convenient for the patient to provide the necessary information. Provide an interactive website with an easy to use, online medical history form and encourage patients to fill out their own medical history at a time convenient for them. This option eliminates scheduling problems, phone tag, and long waits at a clinic. This website can also be used to complete all applicable documentation (release forms, informed consent etc.), educate the patient about their upcoming procedure and discharge process, as well as provide information about their medications and oral intake.
We live in a world of increasing comfort and reliance on Internet based services. Recent surveys indicate that around 74 percent of American adults now use the Internet on a regular basis for things like banking, education, and information gathering.13 Technically savvy consumers prefer to take more control over their own service.
Behind the online form, a best practice model should implement algorithm driven, standardized anesthesia guidelines. The online system should be designed so that it is extremely easy to add or edit the anesthesia guidelines. Some systems may also support stored surgeon preferences as well as intelligent patient acuity assessment. By designing the system to consistently and automatically apply these anesthesia guidelines to every patient, it reduces the risk of human error in ordering diagnostic testing while reducing the system’s reliance on expensive clinical staff.
At this point the patient’s medical history has been captured and a list of recommended diagnostic tests has been generated (except for patients who are unable or unwilling to go online which is addressed below). All of this has been accomplished without the intervention of clinical personnel.
As a final step in the data capture process, a trained clinician assesses each patient’s medical history to assure that the data is complete, makes sense and that the anesthesia guidelines have been appropriately applied. This clinician/screener should also look for anomalous situations not covered by the anesthesia guidelines. If any questions arise, the clinician/screener will call the patient to clarify or expand on the information. If the pre-surgical screening highlights certain risks, then subsequent specific laboratory tests can be run.
For patients who are unable or unwilling to fill out the form online, a team of trained, non-clinical screeners would call the patient, conduct the interview and simultaneously enter the data into the online form. This assures standardized application of the anesthesia guidelines and brings the data into the consistent online data stream. Each of these patients will be then reviewed by the clinician/screener.
An important part of this model is the development and implementation of a comprehensive management system to track all patients by date of surgery. This system should provide a dashboard view of all patients to assure that all screenings and testing is completed prior to surgery.
With consistent data capture into a digital format, distribution of information across all stakeholders is simplified. Standardized reports pre-filled with the appropriate data for anesthesia, nursing assessment, the surgical facility, and surgeons’ offices can be printed and sent via secure fax or email. Duplicative efforts are minimized and consistent data leads to increased integration across the enterprise.
Further, test results and other documentation necessary for the completed chart can be attached to the online record allowing centralization of all data and universal data access.
Business process outsourcing
The increasing costs of Medicare and other public health programs are being shifted to hospitals and surgery centers. Health care providers are receiving lower reimbursements for patient care while also facing increased demands by patients for better care. In response, many health care providers are employing outsourcing solutions to combat rising costs, as well as to address new technology requirements and an ever-changing legal and regulatory environment. Business Process Outsourcing (BPO), with an estimated annual growth rate of more than 10 percent, is one of the fastest growing solutions medical facilities are utilizing to combat these increasing costs. When outsourcing is handled correctly, many executives report that their control over outsourced functions is better than their control over in-house operations.14
To our knowledge, only one company is currently offering the pre-surgical screening service model described above. We expect that the industry is in a startup phase, similar to medical transcription services 10 years ago. In time, we believe that outsourcing of the pre-surgical screening process will become the norm.
Conclusion
The pre-surgical screening model suggested here assures that up to 100 percent of patients will be screened. It provides a better, more convenient experience for the patient while re-tasking clinical resources where they are most effective. It can significantly reduce same-day cancellations and delayed starts while improving the timeliness of data capture and distribution. It facilitates a higher level of integration across the facility, improves patient safety and reduces staff frustration. All of this leads to better operating margins and a better relationship with the community.
While we believe that the intelligent online form is a critical factor, some facilities may choose to initially implement the model without the online form. Effective use of management tools and appropriate tasking of resources based on skill sets will go a long way toward achieving the desired result.
Pre-surgical screening involves far more than simply gathering health histories from patients. It is an integral part of customer service and safety for all surgical patients. From basic patient education to data flow management, a good pre-surgical process offers many benefits to both the patient and the surgical facility. However, to perform at its best, the screening process needs to take advantage of current available technology and new business concepts. A secure, convenient, easy-to-use, fully integrated online screening service enables the screening process to occur more easily, while a comprehensive business service ensures effective completion of the process. The future of Pre-Surgical Screening is here today and it lies in a technology-driven, comprehensive approach to this vital part of surgical care.
Learn more about SurgiScreen.
