Since two physicians opened the first modern day surgery center in 1970 in Arizona as a high quality, lower cost alternative to inpatient hospital surgery care, Ambulatory Surgery Centers (ASCs) have transformed the surgical landscape.
Delivering exceptional outcomes and exceedingly high patient satisfaction scores at substantially lower costs, ASCs are arguably one of the greatest values in medicine. Comparative data involving over 1,000,000 surgeries performed in ASCs in 2015 – 2016 from the California Ambulatory Surgery Association (CASA) indicate an ASC post-operative surgical site infection rate six times lower than hospital outpatient surgery departments (HOPD). CASA’s benchmarking reports on fundamental quality indicators including infection rates, emergency room visits and readmissions provide increased transparency to patients seeking surgical services.
California, the nation’s most populous state, has embraced the ASC, and now is home to more than 760 facilities that are known for pioneering new surgical methods, efficient reimbursement strategies, excellent outcomes, and
exceptional patient care1. Championing the success and growth of ASCs in the state is CASA. Founded in 1988, CASA is recognized as a leader in the outpatient surgery educational field, providing outcome data, operational comparisons, benchmarking and best practices to ASC managers, healthcare professionals, regulators and the public.
In this report, we will review CASA’s benchmarking results and compare them with similar HOPD data. We will also review the medical benefits available to patients who select an ASC for their care, examine the cost savings that ASC patients benefit from, and discuss next steps needed to further develop a universal method of benchmarking.
CASA Benchmarking
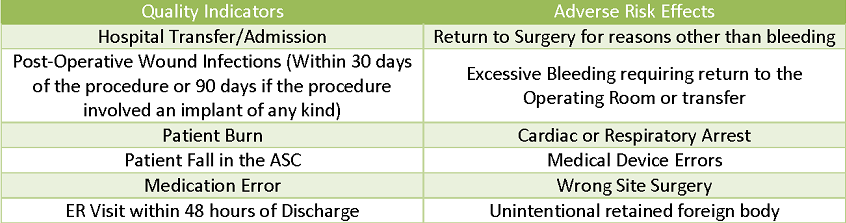
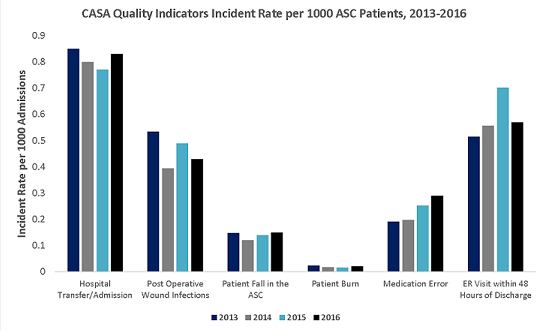
CASA collected data from 147 participating ASCs throughout California. These ASCs performed 1,041,000 surgical cases in 2015 and 2016. The participating ASCs represent urban and rural regions of California and range in size from centers with fewer than 1,000 to more than 15,000 cases. They include 100% physician owned and managed ASCs, those partnering with regional and national management firms and those affiliated with large healthcare systems. Data is self-reported, and although some data may be reported to state agencies (i.e. major complications requiring readmission), it has otherwise not been independently verified. The CASA Benchmarking Report creates a measurement standard through 12 distinct metrics grouped into two categories, Quality Indicators and Adverse Risk Events. Quality Indicators measure events that an ASC can actively work to control, such as patient burns, falls, medication errors and post-operative complications. Adverse Risk Events focuses on improving patient care and the ASC risk management protocol. These data categories are similar to the classifications used by the Centers for Medicare and Medicaid Services (CMS) in their national quality measurement program, Ambulatory Surgical Center Quality Reporting (ASCQR). ASCQR measures Medicare certified ASCs in ten categories. ASCs are required to report patient burns, falls, hospital transfers and hospital admissions to CMS since 2012. CMS utilizes these quality indicators to determine a portion of payment rates to ASCs2.
Increased Focus on Key Measurements
Commercial, federal and state payers are increasingly focused on three key outcome measures--hospital transfers or readmissions, emergency room visits within 48 hours of discharge and infection rates—as quality of care markers. The ASC should routinely monitor these outcomes and compare their performance with industry benchmarks.
When compared to some large studies of hospital outpatient departments (HOPD), the ASC demonstrates superior quality of performance. This is evidenced in post-operative wound infection rates, which CASA Benchmarking identified as occurring .460 per 1000 surgeries ( 412 occurrences per 896,232 patients). An eight state 2014 study of patients receiving outpatient surgery in hospitals, published by the Agency for Healthcare Quality and Research
(AHRQ) found 877 patients out of 280,000 suffered from post-operative treatment for surgical site infection requiring hospitalization. This is an infection rate ratio of 3.09 of every 1,000 or over six and one half times greater than the ASC rate reported by CASA. These results may not be entirely comparable as the studies were not adjusted to reflect patient acuity levels. The differences are nonetheless remarkable and at a minimum, merit additional appropriately designed and controlled research studies. Outcome data comparing the results of identical surgery on patients with similar medical conditions must become transparent to consumers, empowering them to make informed decisions regarding their healthcare options.
Similar to the surgical site infection rate studies on patients receiving outpatient surgery in HOPDs and ASCs, the ASCQR benchmarking program provides a valuable method for measuring performance in the ASC. To generate
greater transparency to patients and the public, ASCQR should consider evolving into a universal management tool, comparing patient outcomes focusing on similar surgeries across all providers and facilities. This increased level of transparency will give patients and payers more information creating a much needed consumer driven open market system in healthcare.
ASC Cost Savings
Commercial payers recognize the superior outcomes and cost savings provided by the ASC. ASCs save patients and employers an estimated $38 billion per year3. Additionally, only 48% of procedures that could be performed in an ASC are actually scheduled there instead of a HOPD, thus suggesting an annual $41 billion opportunity for additional savings2
According to a 2014 report published by the Office of the Inspector General, Medicare saved an estimated $7 billion between 2007 and 2011 and could potentially save an estimated $12 billion during 2012and 2016 due to cost savings found through operational efficiencies and clinical performance in ASCs not found in HOPDs. CASA and other leaders in the ASC industry are at the forefront of promoting transparency in infection rates and other clinical outcome data, patient satisfaction scores and cost, potentially assisting patients consumers and taxpayers save billions of dollars annually4.
Conclusion
Patient data outcomes collected by CASA, although important, are only preliminary. Future benchmarking will evolve and become ever more meaningful as it is adjusted for patient acuity, separated by procedure type, and further refined with subsequent years of analytic design experience.
ASCs have a very rich 47 year history in the US of providing excellent care at affordable prices. As the need to optimize quality and cost becomes even more paramount, ASCs are poised to generate radical changes in how healthcare is delivered in the years ahead. The ASC will continue to capture greater market share as the value to patients, insurers, and the government is more fully recognized. This will help mitigate the upward march of unsustainable healthcare costs that threaten to undermine the federal budget. ASCs are well positioned to be at the forefront in providing transparent pricing and outcomes to the American public. CASA benchmarking efforts are leading this charge.
About the Author
Thomas D. Wilson is a Principal with Global 1, CEO of Monterey Peninsula Surgery Centers and a Principal with Convergent Same Day Surgery Solutions.
1Number of ASC per State. Ambulatory Surgery Center Association. Retrieved January 3, 2017, from http://www.advancingsurgicalcare.com/whatisanasc/numberofascsperstate
2”ASC Quality Reporting.” Centers for Medicare & Medicaid Services. 08 Dec. 2016. Web. 01 Feb. 2017
3Healthcare Bluebook and HealthSmart. Commercial Insurance Cost Savings in Ambulatory Surgery Centers. Retrieved January 2, 2017, from http://www.advancingsurgicalcare.com/advancingsurgicalcare/reducinghealthcarecosts/costsavings/healthcarebluebookstudy
4Munnich E, Parente S. Procedures Take Less Time at Ambulatory Surgery Centers, Keeping Costs Down and Ability to Meet Demand Up. Health Affairs, 33(5), May 2014
The views, opinions and positions expressed within these guest posts are those of the author alone and do not represent those of Becker's Hospital Review/Becker's Healthcare. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them.

