Editor's note: This article by Tony Mira, president and CEO of Anesthesia Business Consultants, an anesthesia & pain management billing and practice management services company, originally appeared in Anesthesia Business Consultants eAlerts, a free electronic newsletter. Sign-up to receive this newsletter by clicking here.
Summary
The proposed Medicare Fee Schedule rule contains the perennial threat of a 27 percent cut in payments to physicians based on the SGR compounded by an approximate three percent reduction for anesthesia services. Initial implementation of the Value-Based Payment Modifier (in 2015) is also featured.
The most significant change for anesthesia and pain medicine practices in the proposed Medicare Fee Schedule rule for 2013 (NPRM), released on July 6, 2012, was the proposal to allow nurse anesthetists to perform chronic pain services without physician supervision in those states that include such services in the scope of practice of nurse anesthesia. As noted in last week's Alert, the 765-page NPRM contains many other potential changes. Highlights appear below.
1. Medicare payment rates in 2013. It comes as no surprise that the 27 percent cut mandated by the Sustainable Growth Rate formula remains in place for now and will take effect on Jan. 1, 2013, if Congress fails to act. Fear of the economic cliff that the entire country faces with mandatory spending reductions and the expiration of tax cuts early next year will undoubtedly affect how Congress deals with the SGR for 2013; what we cannot predict now is how.
On top of the 27 percent SGR cut — if there is one — anesthesia services are expected to be reduced by about three percent, and interventional pain management services by one percent. Most of the decrease results from changes to the relative values for various services, and in particular, to the phase-in of rebased practice expense values. The remainder is attributable to a new shift of the pool of Medicare funds to primary care.
CMS has proposed a new benefit in the NPRM, a "postdischarge transitional care management" service that would include telephone or electronic communication with a patient within two business days of discharge, medical decision-making of moderate or high complexity, and a face-to-face visit with the patient within 30 days following discharge to the community. The service would pay physicians roughly $95 if current rates were implemented in 2013.
Total Medicare payments to family physicians could increase seven percent and fees for other physicians providing primary care could rise three to five percent. Anesthesia and pain management do not bear the cost of the postdischarge transitional care service alone, of course. Other specialties face prospective cuts of as much as 14 percent, in the case of radiation therapy, on top of the 27 percent SGR reduction. Cardiology, vascular surgery and interventional radiation would see a three percent drop, like anesthesiology, if the NPRM were to be finalized in its present form, using its present data.
2. Value-based payment modifier. Introduced in the Affordable Care Act, the value-based payment modifier as outlined in the NPRM could penalize physicians practicing in groups of 25 or more eligible professionals who do not report quality-of-care measures or who are deemed to provide lower-quality care than their peers. In 2015, physicians may see positive (bonus) or negative (penalty) adjustments to their Medicare payments depending on their relative performance on certain cost and quality parameters during 2013. Beginning in 2017, the VBM will apply to all physicians and not just to those practicing in larger groups.
The good news is that anesthesiologists and others who successfully participate in the Physician Quality Reporting System will be able to report a VBM that is equivalent to "nothing done" in the sport of fencing—there will be no payment adjustment upward or downward. Physicians who do not report quality measures under the PQRS would have their pay cut by 1.5 percent in 2015, and groups of 25 or more eligible professionals who do not report PQRS measures would see an additional one percent reduction.
Larger physician groups that do participate in PQRS could elect to have their pay adjusted by the modifier under a quality-tiering approach. Physicians who meet certain quality minimums and contain patient costs could be eligible for payment increases of two percent, but those with lower quality and higher costs per patient could see their pay reduced by one percent (despite successful participation in the PQRS).
The dollar amount of potential bonuses cannot be established in advance because the VBM will operate in budget neutral fashion. The relative adjustments are described in CMS' VBM fact sheet accompanying the proposed rule thus:
In order to achieve the legislatively-mandated budget neutrality for the program, positive adjustments to groups of physicians would be offset by negative adjustments to other groups of physicians. Since the total sum of downward adjustments is unknown at this time, CMS is not proposing specific upward payment amount percentage. Rather, as shown in the table below, CMS is proposing to give groups that are high quality and low cost the highest upward adjustment. The value of "x" will depend on the total sum of negative adjustments in a given year. In addition, to ensure that the Value Modifier encourages physicians to care for the severely ill and beneficiaries with complicated cases, CMS is proposing an additional upward payment adjustment for groups of physicians furnishing services to high risk beneficiaries.
Proposed Calculation of the Value Modifier using the Quality-Tiering Approach
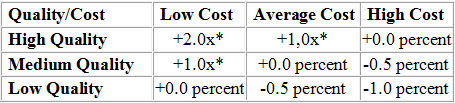
* Eligible for an additional +1.0x if reporting clinical data for quality measures and average beneficiary risk score in the top 25 percent of all beneficiary risk scores.
3. PQRS. There are no new measures for anesthesia.
For 2013 and 2014, CMS proposes to include a total of 264 individual measures, including proposals to align the PQRS measures that would be available for EHR-based reporting with the measures available for reporting under the EHR Incentive Program. In addition, CMS is proposing to bring the total number of measures groups for reporting to twenty-six. CMS also is proposing lower reporting thresholds, a move that would make it easier for physicians to meet PQRS requirements. For instance, groups of 2-99 eligible professionals, and not just those with 25 or more EPs, would be able to use the claims, registry, and EHR-based reporting mechanisms. The minimum number of patients needed to report PQRS measures groups through an approved registry would be lowered to 20 in 2013 from 30 in 2012. The CMS PQRS fact sheet provides further information.
4. Other proposed changes This summer's proposed fee schedule rule contains more policy, as opposed to payment computation, proposals than we typically see. Some others include additional Multiple Procedure Payment Reductions (MPPR) and an expanded list of approved Medicare telehealth services. We continue to review the 765-page NPRM in detail and will be sure to keep you advised of significant developments.
Learn more about Anesthesia Business Consultants.
Related Articles on Anesthesia:
CMS Creates EHR Exemption for Anesthesiologists
AcelRx Begins Final Phase of Testing for Patient-Controlled Analgesia System
NorthStar Anesthesia in Texas to Add Three Physicians to National Team
Summary
The proposed Medicare Fee Schedule rule contains the perennial threat of a 27 percent cut in payments to physicians based on the SGR compounded by an approximate three percent reduction for anesthesia services. Initial implementation of the Value-Based Payment Modifier (in 2015) is also featured.
The most significant change for anesthesia and pain medicine practices in the proposed Medicare Fee Schedule rule for 2013 (NPRM), released on July 6, 2012, was the proposal to allow nurse anesthetists to perform chronic pain services without physician supervision in those states that include such services in the scope of practice of nurse anesthesia. As noted in last week's Alert, the 765-page NPRM contains many other potential changes. Highlights appear below.
1. Medicare payment rates in 2013. It comes as no surprise that the 27 percent cut mandated by the Sustainable Growth Rate formula remains in place for now and will take effect on Jan. 1, 2013, if Congress fails to act. Fear of the economic cliff that the entire country faces with mandatory spending reductions and the expiration of tax cuts early next year will undoubtedly affect how Congress deals with the SGR for 2013; what we cannot predict now is how.
On top of the 27 percent SGR cut — if there is one — anesthesia services are expected to be reduced by about three percent, and interventional pain management services by one percent. Most of the decrease results from changes to the relative values for various services, and in particular, to the phase-in of rebased practice expense values. The remainder is attributable to a new shift of the pool of Medicare funds to primary care.
CMS has proposed a new benefit in the NPRM, a "postdischarge transitional care management" service that would include telephone or electronic communication with a patient within two business days of discharge, medical decision-making of moderate or high complexity, and a face-to-face visit with the patient within 30 days following discharge to the community. The service would pay physicians roughly $95 if current rates were implemented in 2013.
Total Medicare payments to family physicians could increase seven percent and fees for other physicians providing primary care could rise three to five percent. Anesthesia and pain management do not bear the cost of the postdischarge transitional care service alone, of course. Other specialties face prospective cuts of as much as 14 percent, in the case of radiation therapy, on top of the 27 percent SGR reduction. Cardiology, vascular surgery and interventional radiation would see a three percent drop, like anesthesiology, if the NPRM were to be finalized in its present form, using its present data.
2. Value-based payment modifier. Introduced in the Affordable Care Act, the value-based payment modifier as outlined in the NPRM could penalize physicians practicing in groups of 25 or more eligible professionals who do not report quality-of-care measures or who are deemed to provide lower-quality care than their peers. In 2015, physicians may see positive (bonus) or negative (penalty) adjustments to their Medicare payments depending on their relative performance on certain cost and quality parameters during 2013. Beginning in 2017, the VBM will apply to all physicians and not just to those practicing in larger groups.
The good news is that anesthesiologists and others who successfully participate in the Physician Quality Reporting System will be able to report a VBM that is equivalent to "nothing done" in the sport of fencing—there will be no payment adjustment upward or downward. Physicians who do not report quality measures under the PQRS would have their pay cut by 1.5 percent in 2015, and groups of 25 or more eligible professionals who do not report PQRS measures would see an additional one percent reduction.
Larger physician groups that do participate in PQRS could elect to have their pay adjusted by the modifier under a quality-tiering approach. Physicians who meet certain quality minimums and contain patient costs could be eligible for payment increases of two percent, but those with lower quality and higher costs per patient could see their pay reduced by one percent (despite successful participation in the PQRS).
The dollar amount of potential bonuses cannot be established in advance because the VBM will operate in budget neutral fashion. The relative adjustments are described in CMS' VBM fact sheet accompanying the proposed rule thus:
In order to achieve the legislatively-mandated budget neutrality for the program, positive adjustments to groups of physicians would be offset by negative adjustments to other groups of physicians. Since the total sum of downward adjustments is unknown at this time, CMS is not proposing specific upward payment amount percentage. Rather, as shown in the table below, CMS is proposing to give groups that are high quality and low cost the highest upward adjustment. The value of "x" will depend on the total sum of negative adjustments in a given year. In addition, to ensure that the Value Modifier encourages physicians to care for the severely ill and beneficiaries with complicated cases, CMS is proposing an additional upward payment adjustment for groups of physicians furnishing services to high risk beneficiaries.
Proposed Calculation of the Value Modifier using the Quality-Tiering Approach
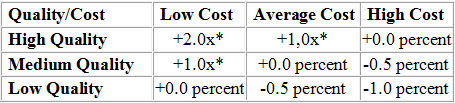
* Eligible for an additional +1.0x if reporting clinical data for quality measures and average beneficiary risk score in the top 25 percent of all beneficiary risk scores.
3. PQRS. There are no new measures for anesthesia.
For 2013 and 2014, CMS proposes to include a total of 264 individual measures, including proposals to align the PQRS measures that would be available for EHR-based reporting with the measures available for reporting under the EHR Incentive Program. In addition, CMS is proposing to bring the total number of measures groups for reporting to twenty-six. CMS also is proposing lower reporting thresholds, a move that would make it easier for physicians to meet PQRS requirements. For instance, groups of 2-99 eligible professionals, and not just those with 25 or more EPs, would be able to use the claims, registry, and EHR-based reporting mechanisms. The minimum number of patients needed to report PQRS measures groups through an approved registry would be lowered to 20 in 2013 from 30 in 2012. The CMS PQRS fact sheet provides further information.
4. Other proposed changes This summer's proposed fee schedule rule contains more policy, as opposed to payment computation, proposals than we typically see. Some others include additional Multiple Procedure Payment Reductions (MPPR) and an expanded list of approved Medicare telehealth services. We continue to review the 765-page NPRM in detail and will be sure to keep you advised of significant developments.
Learn more about Anesthesia Business Consultants.
Related Articles on Anesthesia:
CMS Creates EHR Exemption for Anesthesiologists
AcelRx Begins Final Phase of Testing for Patient-Controlled Analgesia System
NorthStar Anesthesia in Texas to Add Three Physicians to National Team

