Overview
Raleigh Orthopaedic Surgery Center (ROSC) opened in 2013 as a single-specialty ambulatory surgery center (ASC) affiliated with UNC Rex Healthcare in Raleigh, North Carolina. Both the hospital and the ASC are renowned for their strong surgical services, and ROSC has developed a comprehensive strategy for achieving same-day joint surgery with outstanding results.
NAPA anesthesiologist Thomas J. Monaco, MD, joined ROSC at its opening and soon became the anesthesia director. Although he is not an owner in the joint venture, Dr. Monaco brings an ownership mentality to his role, which he continues to hold. His focus on hiring service-oriented anesthesia clinicians, fostering a collaborative culture, and resource stewardship contributes to a positive workplace environment where everyone is working toward shared goals. Metrics for overall satisfaction with anesthesia are routinely reported to be above 95%.
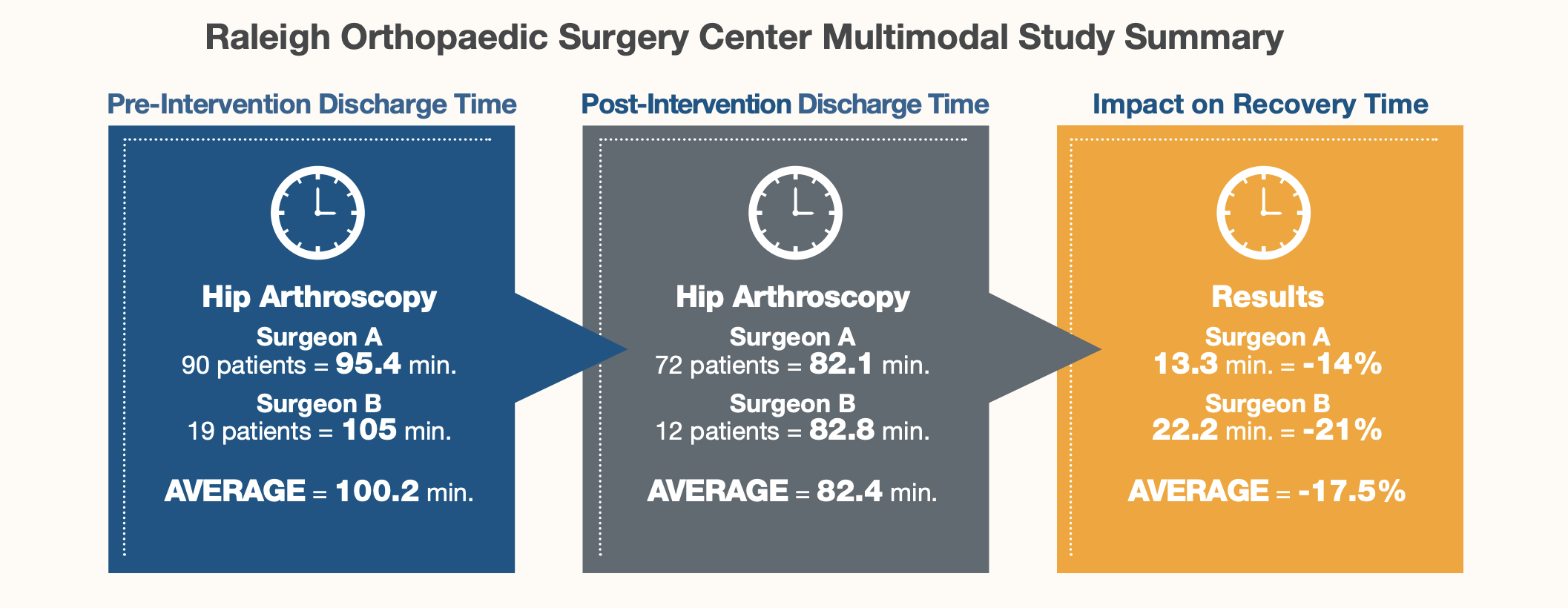
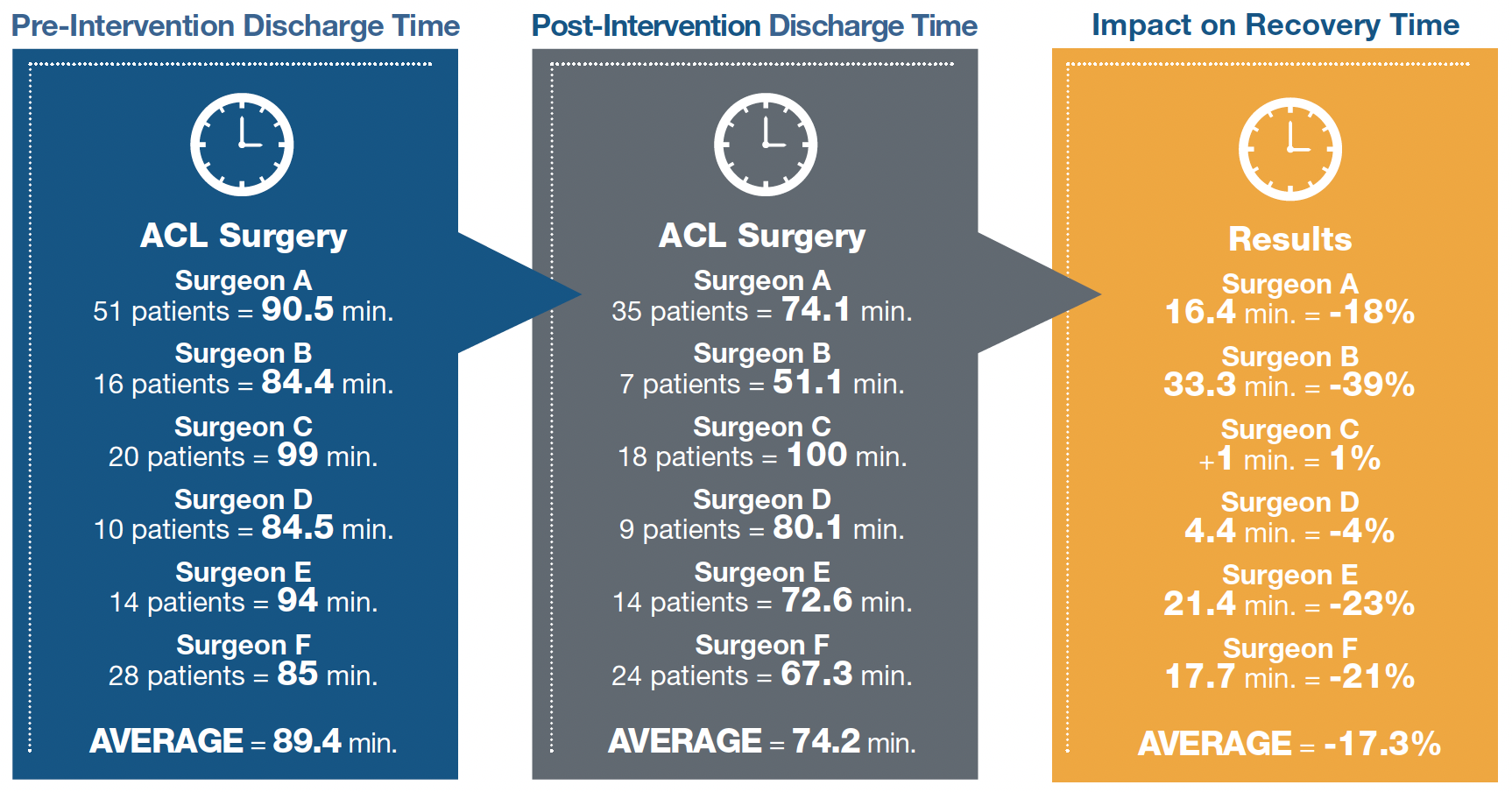
A culture built on an aligned vision facilitates change management. When staff noticed that patients having hip arthroscopy and anterior cruciate ligament (ACL) surgeries were experiencing more pain and postoperative nausea and vomiting (PONV) than total joint patients, delaying the patients’ recovery, they asked Dr. Monaco if he could find a solution. With the surgeons’ collaboration, the anesthesia team developed an expanded preoperative, multimodal pain management strategy that proved to deliver measurable success. Analytic evidence for the six-month periods prior to and after this intervention showed that with the new protocol, patients received less intravenous (IV) opioids, and had less PONV and pain, enabling them to spend less time in the post-anesthesia care unit (PACU) and progress more quickly to discharge.
Situation
NAPA anesthesiologists and certified registered nurse anesthetists (CRNAs) at ROSC work closely with their clinical colleagues to offer orthopedic patients a safe, same-day surgical experience. Highly experienced, the team conducts rigorous preadmission reviews to minimize the risk of day-of-surgery cancellations, and their perioperative focus provides most patients, even for complex cases, with short postoperative stays in the PACU.
The anesthesia department is also heavily invested in being a dedicated partner to ROSC. Dr. Monaco participates in value-based purchasing and continually seeks to promote profitability by controlling expenditures for anesthesia equipment and supplies. As a team, the anesthesia clinicians take a hands-on approach to meeting operational objectives and are recognized for helping to advance the ASC’s clinical and financial goals.
This level of support over many years has created a culture characterized by trusting relationships and open communication. Thus, when nurses noticed that only the hip and ACL patients had prolonged PACU times, they brought the issue to Dr. Monaco. He recognized that patients in these challenging groups were experiencing high amounts—and a higher incidence— of PONV, which was delaying their recovery. The greater prevalence of PONV was attributed to the administration of IV opioids.
Solution
Based on current evidence, Dr. Monaco suggested making several changes to pain medications that were typically administered preoperatively, expanding a multimodal approach that reduced the use of fentanyl and oxycodone. He also changed the IV administration of ketorolac, a nonsteroidal anti-inflammatory drug, from the operating room to the PACU.
Dr. Monaco presented his plan and supporting data to the surgeons, to secure their collective buy-in for this new process.
Results
After implementing the new pain protocol for hip and ACL patients, their recovery times were substantially reduced, becoming more consistent with those experienced by the general ROSC patient population. A subsequent outcomes study of the six-month periods pre- and post-intervention showed that without changing anything else in the surgical and anesthetic management of these patients, they felt better and were able to go home sooner, improving satisfaction for patients and their surgeons.
Because reducing PACU time by even a matter of minutes was important to the ROSC surgeons, it was important to the NAPA anesthesia team. NAPA’s anesthesia clinicians are highly focused on helping ASCs optimize resource utilization by continuously examining clinical processes and operational efficiencies. Being a strong anesthesia partner means supporting institutional goals at every level and adding value at every opportunity.
Click here to contact NAPA or call 833-OR1-TEAM to learn more about driving results at your outpatient center.

